Screening policies to detect chronic kidney disease in children have been widely debated. Now, extensive evaluation of the costs of screening versus the quality-adjusted life years gained through the screening program suggests it is cost effective in Japan.
©︎ Crystal Light― stock.adobe.com/jp
Screening for kidney disease in asymptomatic children has attracted debate, with evidence accruing both for and against the policy in different parts of the world. To assess the cost effectiveness of the approach, Keio University's Kimiko Honda and Rei Goto leveraged past data on kidney screening in Japan where the policy has been in place for over 50 years. "I started this research because as a pediatrician I want to clarify the value of pediatric care from a societal perspective, including costs." explains Honda. "And, with the guidance of Professor Goto at the Graduate School of Business Administration―who is also a trained medical doctor―I was able to pursue this challenging area of research."
School urinary screening in Japan is conducted using a dipstick test for traces of hematuria and proteinuria in a urine sample collected at home. Testing is mandatory for all students in schools and screening rates in elementary and junior schools are close to 100%. A second test is conducted for those with positive test results, followed by a full medical examination and treatment where necessary if the second test is also positive.
Honda and her colleagues took data from previous studies and clinical trials to identify parameters such as probabilities for the annual incidence of nephropathy
caused by deposits of the protein immunoglobulin (IgA nephropathy:IgAN, the most common form of kidney disease), severe IgAN, developing end stage kidney disease without treatment,
or remission with treatment among others.
Based on these statistics, they then calculated the probability for a hypothetical cohort of 1,000,000 individuals being in one of 5 states (No IgAN, mild IgAN, severe IgAN, asymptomatic hematuria and deceased) and transitioning between states from the age of 6 until they reach 120 or the end of their lifetime.
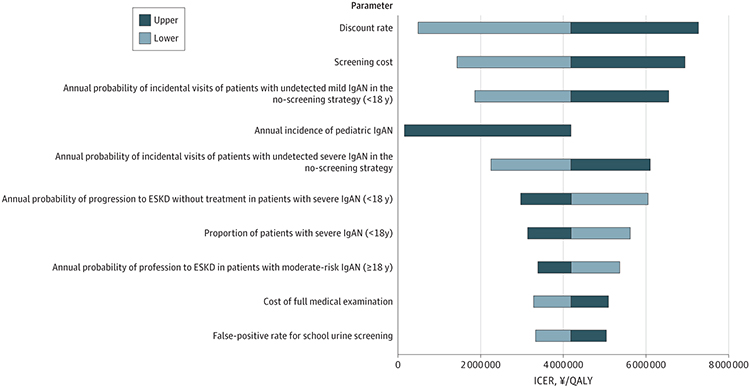
Fig. 2 from the paper
Tornado Diagram of 1-Way Sensitivity Analysis in Base-Case Analysis
(https://doi.org/doi:10.1001/jamanetworkopen.2023.56412) is licensed under CC-BY
The researchers took into account the costs of screening, such as urine containers and other testing paraphernalia, as well as follow-up examinations and treatment. In this context, a diagnosis of asymptomatic hematuria is positioned as a negative outcome because of the cost of the tests and examinations with no potential benefit from its detection. Using their hypothetical cohort they could also examine the cost-effectiveness impact of scenarios where the frequency of screening was reduced or the age at which screening began increased.
The researchers set a threshold incremental cost effectiveness ratio of ¥7,500,000 (US$70,093) per quality adjusted life year as this is used for pediatric diseases in Japanese official health technology assessments. From their analysis the researchers calculated an incremental cost effectiveness ratio for the current screening program of ¥4,186,642 (US$39,127) per quality-adjusted life year, well below that threshold. "Screening costs, annual probability of detecting cases outside screening, and IgAN incidence were key factors associated with the program's cost-effectiveness," says Honda.
Honda notes that the results cannot be directly applied universally because the incidence of IgAN varies worldwide, with higher cases in Asia, particularly Japan (4.5-9.9 per 100,000), than Europe (0.2 per 100,000) or the United States (0.3-1 per 100,000).
Honda concludes that "Japan's 12-year school urinalysis program has been effective in terms of reducing the number of ESKD cases and has been cost-effective in focusing on early detection and treatment of IgAN."
Published online 8 July 2024
About the researcher

Kimiko Honda ― Project Assistant Professor (Non-tenured)
Graduate School of Health Management
Kimiko Honda graduated from Showa University School of Medicine
in 2003 and has been practicing as a pediatrician and pediatric
nephrologist. She earned a Master of Public Health degree from the
University of Tokyo School of Public Health in 2021 and
is expected to obtain her PhD from the Keio University Graduate School of Health
Management in 2024. Her areas of expertise include
pediatrics, pediatric nephrology, economic evaluation,
and quality of life in children with chronic diseases.

Rei Goto ― Professor
Graduate School of Business Administration
Rei Goto graduated from the Kyoto University Faculty of Medicine
in 1998 and earned a PhD in Economics from the Kyoto University
Graduate School of Economics. He is currently a Professor at the Keio University
Graduate School of Business Administration.
Since 2019, he has been concurrently serving as a Professor at the
Graduate School of Health Management. His research interests are
in health economics, health policy, health technology assessment,
and behavioral economics.
Links
Reference
- Honda, K., Akune, Y. & Goto, R. Cost-Effectiveness of School Urinary Screening for Early Detection of IgA Nephropathy in Japan. JAMA. Netw. Open 7, e2356412 (2024). | article