Discovery of a protein fragment gives rise to a new strategy for harnessing the immune system against leukemia
Published online 17 March 2016
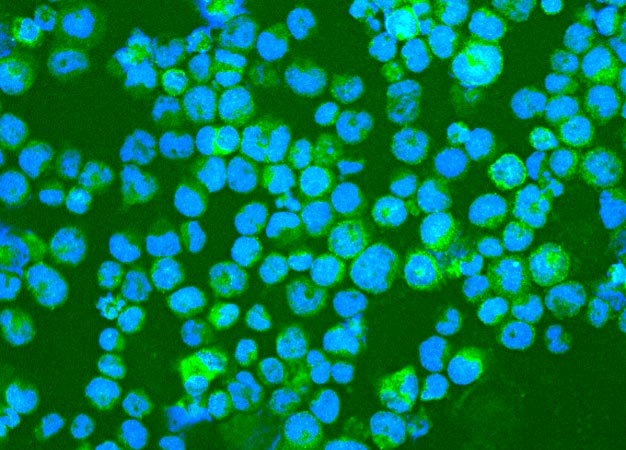
Leukemia cells expressing the surface protein PEPP2 (labeled bright green) that immune cells in the body can recognize.
© 2016 Maiko Matsushita, Keio University
A protein fragment newly identified by Keio researchers1 and expressed in leukemia cells points to a target for developing novel immunotherapies to combat the deadly blood cancer.
Scientists have known for more than a decade that many tumor cells, and cells from leukemia blood cancers in particular, express a protein called PEPP2 that can trigger an immune response (see image). However, it was unclear what part of the protein specialized immune cells called killer T cells recognized and latched on to.
A team led by Maiko Matsushita, a hematologist and cancer immunologist at Keio University, went in search of the elusive site on PEPP2 to which white blood cells bind ― a site known as the epitope. They synthesized 24 fragments of the PEPP2 protein. Using immune cells from healthy donors in the laboratory, they singled out one PEPP2 fragment ― a nine amino-acid stretch ― that roused the killer T cells into action.
With this small protein fragment, "we could induce anti-PEPP2 killer T cells with strong activity," Matsushita says. "This encouraged us to believe that this epitope might be useful for many leukemia patients."
To boost the expression of PEPP2 on leukemia cells, and increase the potency of the anti-PEPP2 T cells, Matsushita and her colleagues exposed the leukemia cells to a drug that removes chemical marks from the DNA. These marks, known as methyl tags, restrict gene expression, and the researchers found that the 'demethylating' drug increased levels of PEPP2 expressed in the leukemia cells. The cells were subsequently more vulnerable to attack from killer T cells.
The findings could pave the way for a new therapeutic strategy for combatting leukemia, a disease that kills more than 250,000 people globally each year. Matsushita envisions a scenario in which scientists genetically engineer a patient's own T cells in the laboratory so that they respond to PEPP2 more actively and efficiently. Those cells could then be infused back into the patient together with a drug that takes away the methyl tags from the DNA of the cancerous cells in the body.
The approach would need to be tested in animal models and then in human clinical trials. But if it proves safe and effective, it could greatly benefit patients who don't respond to existing drugs or who experience disease recurrence. "For those patients," Matsushita says, "immunotherapy targeting PEPP2 might be a good treatment option, since PEPP2 is also expressed in leukemia stem cells, which are one of the reasons for disease relapse."
Reference
- Matsushita, M. et al. Identification of novel HLA-A*24:02-restricted epitope derived from a homeobox protein expressed in hematological malignancies. PLoS ONE 11, e0146371 (2016). | article